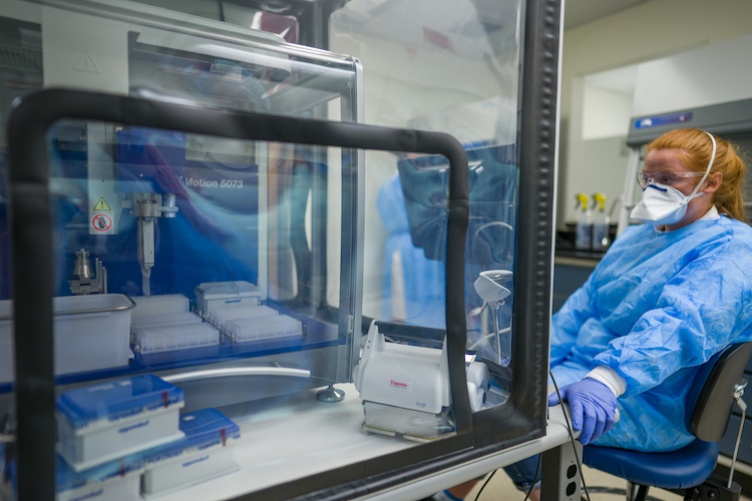
When professor Kelley Thomas turned on the lights in the COVID-19 testing lab on a recent Monday morning, he says there are no words to describe what he felt.
After months of working around the clock with his team to establish the facility, the director of the Hubbard Center for Genome Studies saw that the lab was officially up and running. Students were back on campus. What they’d set out to do was working.
“There’s no practicing this,” says Thomas, who serves as the lab’s scientific director. “You can’t say, ‘send me 4,000 samples so we can try this out.’”
That meant starting off the semester by going from zero to 4,000. As in zero actual tests over the summer months to 4,000 – in a day.
But nothing less than that incredible velocity would suffice. Rick Cote, director of the Center of Integrated Biomedical and Bioengineering Research, is a member of the university planning team responsible for building out the facility. He says that the lab’s capacity to test with scale, precision and efficiency – right from the get-go – was crucial. It provides the timely data that makes essential efforts like contact tracing possible in the first place.
“There’s no practicing this... You can’t say, ‘send me 4,000 samples so we can try this out.’”
“Everyone, often,” Thomas explains is the lab’s unofficial mantra: they need to be able to test everyone on campus – and often.
Early on in the process of developing the lab’s design and protocols, Thomas, Cote and their cohort of experts made the decision to move forward with a specific type of test: RT-PCR, which is short for real-time reverse transcription polymerase chain reaction.
Thomas says that this test is the gold standard in molecular diagnostics because it’s both sensitive and robust. Probes are able to swiftly identify the virus’s fingerprint in a small test sample by binding and copying its unique strands of genetic material. Since the DNA of COVID-19 genes continues to adapt and shift, the test actually looks for three different gene types, bolstering its accuracy.
"It’s like a fingerprint test that uniquely identifies not just the thumb, but also the first and second finger,” Cote explains.
But what do you do with all of that data?
“Have you ever seen 2,000 test samples dumped out of a biohazard bag that’s been carried into the lab by two policemen?” Thomas says. “That’s what happens – twice a day.”
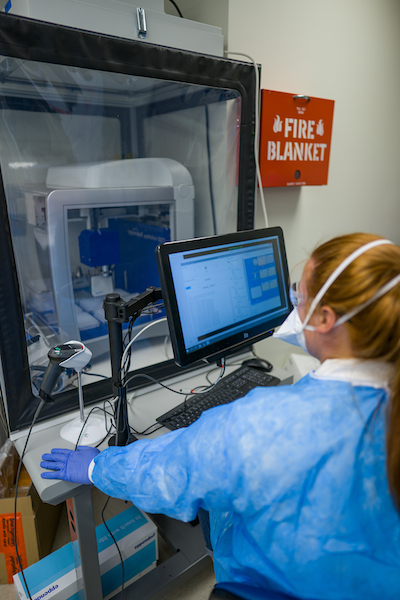
That’s why automating as much of the process as possible was a goal from the very beginning. Computational scientist Anthony Westbrook created the software that scans each test’s barcode and tracks it all the way through. Even with thousands of samples being tested every day, the tracking system allows them to pinpoint a single positive sample.
“This is fundamental,” Thomas says. Of course, there are also robots. Robots for taking the sample out of the tube, for instance, or placing the samples on trays to be tested. “Yeah, the robots are fun,” Thomas says. “But I don’t know where we’d be without the incredibly dedicated staff.”
“It takes the entire UNH ecosystem,” Cote adds.
That includes having a world-class genomics research center right on campus. But it also comes down to the sheer ingenuity and resilience of the many individuals involved every step of the way – like the facilities staff who hoisted not one but two 1,500-pound biosafety cabinets through a window when they wouldn’t fit through the lab door.
Today, Cote says the lab is like a beehive. It’s open from 7 a.m. to 11 p.m. every day, with shifts staffed by a number of recent life sciences alums.
“If UNH is successful in staying open through Thanksgiving, this lab will have played a central role,” Cote says. “We’re proud that UNH has the scientific and technical resources, along with the backing of university and state leadership to implement large-scale testing this fall.”
-
Written By:
Ali Goldstein | CPA