Editor’s note: Supported by a $15.4 million award from the National Institutes of Health, the New Hampshire IDeA Network of Biomedical Research Excellence (NH INBRE) aims to increase the state’s research capacity and the scientific knowledge of its workforce. Leading the coalition is Dartmouth, which oversees the awarding of NH INBRE grants and provides technical support and mentoring to partners in the coalition, including UNH. This is part three of a three-part series that profiles UNH faculty and students who are involved in NH INBRE.
|
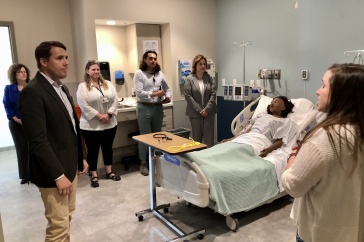
Jenna McCarthy, INBRE Nursing Research Fellow |
UNH student Jenna McCarthy ’13 first heard about NH INBRE’s iSURF-N program three days before the deadline to apply. Her adviser stopped her in Hewitt Hall, handed her an application, and encouraged her to complete it. At first the nursing student was hesitant; all she knew about the program was that it involved conducting clinical research. Then she realized she could either stay at home over the summer or try something new.
“I took a leap of faith – and it paid off hugely,” McCarthy says. “It was so much more than I ever expected going into it. I’m fortunate to have had the opportunity literally dropped in my hands.”
As McCarthy learned, iSURF-N is the “Bench to Bedside” Summer Nursing Research Fellowship Program at Dartmouth-Hitchcock Medical Center in Lebanon. It gives undergraduates a chance to experience many aspects of the research process, from formulating a study question to applying findings to patient care. In keeping with NH INBRE’s goal of boosting the state’s research capacity, iSURF-N aims to increase the number of new nurses who decide to pursue research in their careers.
|
Andrew Quinn, INBRE Nursing Research Fellow |
Last summer, two rising seniors from UNH participated: McCarthy and fellow nursing student Andrew Quinn ’13. Andrew Guilliams ’13, a chemical engineering major, took part in the closely related iSURF, a biomedical research program that places undergraduates in laboratories at Dartmouth’s medical school and in the private sector. Guilliams worked at Mascoma Corporation on an ethanol project.
Among the projects McCarthy worked on with DHMC nursing staff was a study that looked at the progress of children with voiding problems in a bladder and bowel retraining program. Specifically, the study examined whether children who had been diagnosed with neuropsychiatric disorders or who had experienced traumatic events improved more or less than children without psychosocial issues. Her group’s preliminary results, presented on a poster at the NH INBRE annual meeting last July, suggested that neuropsychiatric disorders were more likely to hinder progress than adverse childhood experiences. However, children with psychosocial issues who remained in the program showed greater improvement than those with no psychosocial issues. McCarthy plans to analyze the data further for her senior honors project.
Before beginning the 10-week program, McCarthy thought she’d have a mostly passive role observing others. “I was surprised and glad to find it was the opposite,” she says. “It was much more the case that if I didn’t do my job and collect the data, the project would have gotten nowhere.”
Quinn also found himself immersed in the research process. He worked with the epilepsy team to evaluate an alarm that detects seizures by measuring oxygen saturation and heart rate. They found that this new Patient SafetyNet system identified a frequent seizure type faster than the standard alarm activated by brain waves for seizure activity. (Doctors often take patients off anti-seizure medications so they can learn more about their seizures and determine treatment options; the Patient SafetyNet monitoring informs nurses when seizures occur.) The team concluded that the Patient SafetyNet helps nurses respond more quickly to generalized seizures.
Quinn, who presented these findings at the NH INBRE meeting, plans to continue working with the epilepsy team for school credit. He also has been hired to assist the palliative care team – which works to improve quality of life for terminally ill patients – with a study that looks at the benefits of offering palliative care to patients soon after their diagnoses.
Quinn notes that there’s a move in nursing toward evidence-based practice, which uses research findings to help direct patient care. “My experience this past summer reinforced the necessity to think about everything we do, and it showed me that you can actually influence hospital policy pretty easily at Dartmouth-Hitchcock,” he says. “With both the epilepsy and palliative care studies, we could see the change happening right there.”
Although McCarthy and Quinn plan to begin nursing jobs after graduation, they both think that graduate school may be in their future. “Before this, I don’t think I would have taken that extra step,” Quinn says. “It’s opened up lots of new directions.”
And next summer, McCarthy and Quinn will be back at Dartmouth-Hitchcock, this time coordinating the iSURF-N program for the next group of student researchers.
Originally published by:
UNH Today
Written by Sonia Scherr ’13MFA