Aerobic exercise, which includes activities such as running and walking, conditions the cardiovascular system and builds endurance. Distance running is a popular form of aerobic exercise and a competitive sport where overuse injuries are often a result of training (Wiegand et al., 2019). When runners are injured, they may need to reduce or sometimes stop their training for several weeks to months (Liem et al., 2013). Within only three weeks of stopping training, endurance-trained athletes experience a significant seven percent decrease in maximal oxygen consumption, or the amount of oxygen they take in during maximum effort aerobic exercise. This decrease in oxygen consumption is an indicator of decreased fitness level (Coyle et al., 1984; Neufer, 1989).

Violet Sullivan with one of her research study participants and fellow researcher Amanda Ares.
When recovering from injury, runners may engage in rehabilitation programs to mitigate losses in their aerobic fitness, or detraining (Fredericson et al., 2006). Blood flow restricted (BFR) exercise is a rehabilitative modality that allows individuals to gain fitness benefits while working under lower mechanical loads and intensities (Hughes et al., 2019). As an exercise science major with a love of sports medicine, and as a chronically injured distance runner on the University of New Hampshire’s women’s cross country and track teams, I sought to combine my personal and academic interests by conducting research on this topic for my Honors thesis. With funding from a Summer Undergraduate Research Fellowship (SURF) from the Hamel Center for Undergraduate Research, my objective was to study cardiorespiratory and metabolic responses to low-intensity blood flow restricted running.
Blood flow restriction employs the use of a pressurized cuff or tourniquet around the upper portion of the upper or lower extremities during exercise (Pope et al., 2013). This reduces blood flow, leading to blood pooling and hemodynamic, or blood flow, stress (Staunton et al., 2015; Tegtbur et al., 2020). This added stress makes blood flow restricted exercise difficult to perform, which is why it is done at low intensities. Low-intensity aerobic exercise with blood flow restriction has been shown to increase heart rate, oxygen consumption, and ratings of perceived exertion when compared to the same low-intensity controls without blood flow restriction (Mahoney et al., 2019; Renzi et al., 2010; Silva et al., 2021). This makes it a viable exercise mode for long-distance runners looking to combat cardiorespiratory and endurance losses during detraining periods (Mujika & Padilla, 2001). Previous research on this topic has shown that when compared to high-intensity aerobic exercise, low-intensity blood flow restricted exercise results in lower cardiorespiratory and metabolic responses (Chen et al., 2021; Corvino et al., 2017; Wei et al., 2021). However, this could be due to inadequate comparisons between the type of exercise, intensity, and duration, as most prior studies used interval training for the high-intensity condition (Chen et al., 2021; Corvino et al., 2017; Wei et al., 2021). Because endurance athletes primarily train in continuous bouts of exercise as opposed to high-intensity intervals, further research into these variables is needed.
Therefore, the purpose of this study was to compare participants’ cardiorespiratory and metabolic responses during acute sessions of low-intensity blood flow restricted running with the same responses observed during high-intensity running without blood flow restriction. I hypothesized that cardiorespiratory and metabolic responses including heart rate, oxygen consumption, blood lactate, and ratings of perceived exertion, would be similar across the two different modalities of exercise.

Figure 1. Demographics of the female competitive runners are presented as means + S.D.
Methods
The participants of this study were fifteen healthy female distance runners who I recruited by word of mouth, social media, and local road races. The participant demographics are outlined in Figure 1, showing that they were experienced and competitive distance runners. The participants were each compensated with $40 Runner’s Alley gift cards.
This study consisted of four visits total, attended over approximately two weeks. Working with human subjects in this study, we needed to constantly adapt to participants’ schedule changes and needs, while still meeting the criteria outlined in the study methods. All testing took place in the Robert Kertzer Exercise Physiology Laboratory in New Hampshire Hall at UNH.
In visit one the participant completed the informed consent requirements, and I measured their height, weight, and body composition on an InBody machine (InBody770; California, USA). I then fitted participants with a mask (7450 V2 Series; Kansas, USA) to collect exhaled air, and a heart rate monitor (Polar H10 Heart Rate Sensors) at the sternum. I conducted an incremental maximal oxygen consumption testing protocol on each participant, where they ran on a treadmill (Fitnex Fitness #3020; Texas; USA) while we measured their exhaled air (ParvoMedics TrueOne 2400 Metabolic Measurement System; Utah, USA) and heart rate. This testing determined the participants’ cardiorespiratory endurance, and I used these values to determine the appropriate running speeds for each individual in visits two through four.
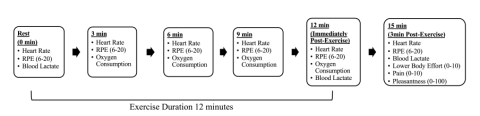
Figure 2. Timeline and measurements obtained during each condition of the experimental trials. RPE, Ratings of Perceived Exertion.
Additionally, I determined each participant’s arterial occlusion pressure (the pressure where no blood is flowing) to designate pressure of the blood flow restriction that would be applied during visits two through four using B Strong cuffs. To do this, the participants wore cuffs on their upper legs, then I placed a doppler ultrasound (Hokanson Inc. MD6 Bidirectional Doppler; Washington, USA) on the participant’s posterior tibial artery in her foot and inflated the cuffs until no pulse was heard. The point where no blood flow was heard determined the arterial occlusion pressure, and this number was used to calculate 50 percent arterial occlusion pressure for the low-intensity blood flow restricted condition in visits two through four. This means the participants would always have blood flowing to their legs during the exercise, though it was restricted to be about half as much as usual, based on the predetermined pressure specific to each participant.
Figure 2 shows a schematic representation of the timeline and measurements obtained during each experimental trial. At least three days after visit one, the participants returned to the lab. In visits two through four, participants underwent three randomly assigned experimental conditions: a controlled low-intensity (40 percent maximal oxygen consumption speed) running, low-intensity blood flow restricted (40 percent maximal oxygen consumption) running, and high-intensity (80 percent maximal oxygen consumption) running. Participants had at least 48 hours of recovery in between these visits.
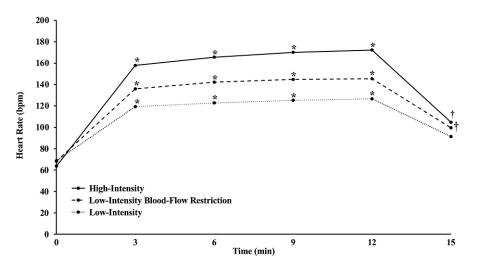
Figure 3. Depicts the mean heart rate (bpm) for each 3-minute increment during the 3 experimental conditions from rest (0mins) to exercise (3, 6, 9, and 12mins) to 3-minute post recovery (15mins). * denotes significantly different between all conditions (p < 0.001), and † denotes significantly different from low-intensity (p < 0.001). Click to enlarge.
The low-intensity control condition consisted of twelve minutes of treadmill running without blood flow restriction cuffs. For the low-intensity blood flow restricted condition, participants first completed a three-minute warm-up walk. We then put the cuffs on participants and inflated the cuffs to the pressure determined during their first visit. After twelve minutes of exercise, we stopped the treadmill and deflated the cuffs immediately. The high-intensity condition consisted of 12 minutes of treadmill running without the cuffs.
The metabolic cart continuously recorded participants’ heart rate and oxygen consumption values throughout each session. Participants self-selected their ratings of perceived exertion on the Borg 6-20 scale, a commonly used scale where six is the easiest effort and 20 is the hardest effort that an individual has experienced. I recorded their ratings of perceived exertion (RPE) at rest, every three minutes, and three minutes post-exercise by having the participants point to the number of their exertion on the RPE poster. We measured blood lactate at rest, immediately after exercise, and three minutes post exercise using a Nova Biomedical Lactate Plus Measurement System to analyze blood from finger sticks. More subjective measures of lower-body effort, pain, and pleasantness of the twelve minutes of running were self-selected by the participants following each session.
The descriptive data from this study were presented as means and standard deviations. The independent variable was the condition (low-intensity blood flow restricted running, high-intensity without blood flow restriction, and a control low-intensity without blood flow restriction). The dependent variables were heart rate, oxygen consumption, blood lactate, and ratings of perceived exertion.
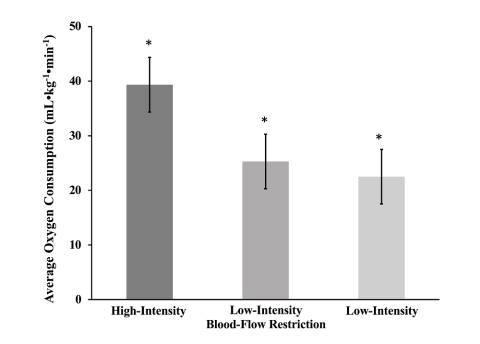
Figure 4. Depicts the mean + S.D. oxygen consumption (mL•kg-1•min-1) during each experimental condition. * denotes statistically different between all conditions (p < 0.001). Click to enlarge.
I analyzed data first by using repeated measures of Analysis of Variance tests to determine significant differences in the cardiorespiratory and metabolic responses between the conditions. Because each participant underwent all three exercise conditions, this was a more vigorous way to test. If I found significant differences, I then used post hoc t-tests with Bonferroni corrections to compare the dependent variables during each condition. I used IBM Statistical Package for the Social Sciences (SPSS) for Mac Version 28 (IBM Corp; Armonk, NY) to analyze the data.
Discussion of Findings
Going into this project, my aim was to see if low-intensity blood flow restricted running could elicit the same cardiorespiratory and metabolic demands as running at a high-intensity without blood flow restriction. Similar to previous studies, my results showed that high-intensity running elicited the greatest acute responses in average heart rates and oxygen consumption, followed by low-intensity blood flow restriction, then the low-intensity control (Figures 3 and 4). Notably, the three-minute post-exercise recovery heart rate for low-intensity blood flow restriction and high-intensity were similar (Figure 3).
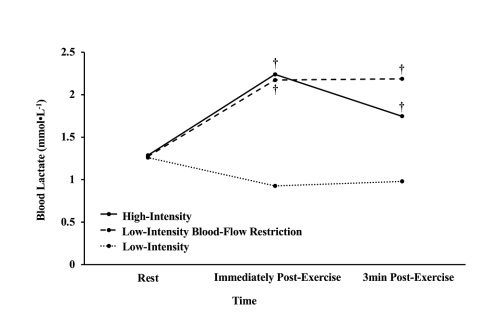
Figure 5. Depicts the mean blood lactate measurements (mmol•L-1) during the 3 experimental conditions from rest (0min) to immediately post (12mins) to 3-minutes post exercise recovery (15mins). † denotes significantly different from low-intensity (p < 0.017). Click to enlarge.
Blood lactate responses (Figure 5) and average ratings of perceived exertion (Figure 6) were also similar in high-intensity and low-intensity blood flow restriction. Additional ratings of perceived exertion for lower body effort, pain, and pleasantness are depicted in Figure 7. The blood flow restriction condition required the most lower body effort, was the most painful, and the least pleasant compared to high- and low-intensity conditions without blood restriction. For pleasantness, high-intensity and the low-intensity control were similar.
Because high-intensity running elicited greater oxygen consumption and heart rate responses than low-intensity blood flow restricted running, this suggests that high-intensity running results in more robust long-term training responses. However, these results also show that if one cannot engage in high-intensity running because of injury and rehabilitation, low-intensity blood flow restricted running could be a feasible alternative in times of decreased training volume and intensity because it does yield some similar responses. Although running with blood flow restriction cuffs at a slow pace is not as physically demanding as faster running without cuffs, someone who is returning to running from injury or needs to run slower could benefit physically from this exercise modality. These results help us better understand the body’s acute response to low-intensity blood flow-restricted running, which will allow us to evaluate this exercise modality in terms of feasibility and application to future training studies on rehabilitation and return to sport protocols.

Figure 6.Depicts the mean + S.D. ratings of perceived exertion for aerobic effort (6-20), lower body effort (0-10), pain (0-10), and pleasantness (0-100). * denotes significantly different between all conditions (p < 0.001), † denotes significantly different from low-intensity (p < 0.001), ‡ denotes significantly different from low-intensity blood-flow restriction (p < 0.001). Click to enlarge.
It’s important to note that all but one of the participants in this study said that they would incorporate blood flow-restricted running into their training if it could help to mitigate losses in fitness, even though the subjects indicated that it was painful and unpleasant. It is equally important to note that the practicality and feasibility of running with blood flow restriction cuffs may not be the same for populations without an urgency to return to sport. Recreational runners may not use blood flow restriction if it is painful and unpleasant, regardless of any potential benefits. Additionally, this study looked at acute responses to low-intensity blood flow-restricted running, and the long-term effects of blood flow restriction training are currently unknown, so there is a need for future training studies. This area of research has the potential to be important to the fields of exercise science and rehabilitative medicine.
Reflection
Following data collection and analysis, I presented my research at the Fall 2022 New England Chapter of American College of Sports Medicine Conference in Providence, RI, where I was selected as a finalist in the Student Investigator Award Competition. This was an incredible experience to share my work, and I’m proud to have won the undergraduate competition. I plan to submit my Honors senior thesis, which is based on this research, to a peer-reviewed journal in the field this spring. I will also present at the UNH Undergraduate Research Conference and at the CHHS Grimes Competition in April.
My goal following UNH is to go to medical school and most likely specialize in physical medicine and rehabilitation with sports medicine. Having the experience of doing research in this field and working with human subjects as an undergraduate student has been a great opportunity. It was fun to build a relationship with many of the subjects while sharing knowledge and an interesting experience with them. I personally would use blood flow restricted running when injured, if it could help mitigate some of the losses in fitness, and I hope that the results of this study can potentially help other runners who are struggling with rehabilitation from injury in the future. I want to continue to do research in medical school and as a professional, and I am so thankful for my undergraduate research experiences at UNH. Performing research and working with Summer Cook, associate professor of kinesiology at UNH, has been the highlight of my undergraduate career.
I would like to thank Dr. Cook for all her help and guidance for the past four years. We’ve been a great team working together. I am very thankful for the help of sophomore REAP student Amanda Ares for her assistance in all my summer testing. Additionally, thank you to Allison Petry and Bilal Chaudhry for helping with my pilot testing. Thank you to the Hamel Center for Undergraduate Research for supporting my projects, especially Mr. Dana Hamel, Patricia M. Flowers ‘45 Scholarship Fund, and Ms. Lynda Banzi. Additionally, thank you to all my participants.
References
Chen, Y.-T., Hsieh, Y.-Y., Ho, J.-Y., & Lin, J.-C. (2021). Effects of Running Exercise Combined With Blood Flow Restriction on Strength and Sprint Performance. Journal of Strength and Conditioning Research, 35(11), 3090–3096. https://doi.org/10.1519/JSC.0000000000003313
Corvino, R. B., Rossiter, H. B., Loch, T., Martins, J. C., & Caputo, F. (2017). Physiological responses to interval endurance exercise at different levels of blood flow restriction. European Journal of Applied Physiology, 117(1), 39–52. https://doi.org/10.1007/s00421-016-3497-5
Coyle, E. F., Martin, W. H., Sinacore, D. R., Joyner, M. J., Hagberg, J. M., & Holloszy, J. O. (1984). Time course of loss of adaptations after stopping prolonged intense endurance training. Journal of Applied Physiology: Respiratory, Environmental and Exercise Physiology, 57(6), 1857–1864. https://doi.org/10.1152/jappl.1984.57.6.1857
Fredericson, M., Jennings, F., Beaulieu, C., & Matheson, G. O. (2006). Stress fractures in athletes. Topics in Magnetic Resonance Imaging: TMRI, 17(5), 309–325. https://doi.org/10.1097/RMR.0b013e3180421c8c
Hughes, L., Rosenblatt, B., Haddad, F., Gissane, C., McCarthy, D., Clarke, T., Ferris, G., Dawes, J., Paton, B., & Patterson, S. D. (2019). Comparing the Effectiveness of Blood Flow Restriction and Traditional Heavy Load Resistance Training in the Post-Surgery Rehabilitation of Anterior Cruciate Ligament Reconstruction Patients: A UK National Health Service Randomised Controlled Trial. Sports Medicine (Auckland, N.Z.), 49(11), 1787–1805. https://doi.org/10.1007/s40279-019-01137-2
Liem, B. C., Truswell, H. J., & Harrast, M. A. (2013). Rehabilitation and return to running after lower limb stress fractures. Current Sports Medicine Reports, 12(3), 200–207. https://doi.org/10.1249/JSR.0b013e3182913cbe
Mahoney, S. J., Dicks, N. D., Lyman, K. J., Christensen, B. K., & Hackney, K. J. (2019). Acute Cardiovascular, Metabolic, and Muscular Responses to Blood Flow Restricted Rowing Exercise. Aerospace Medicine and Human Performance, 90(5), 440–446. https://doi.org/10.3357/AMHP.5258.2019
Mujika, I., & Padilla, S. (2001). Cardiorespiratory and metabolic characteristics of detraining in humans. Medicine and Science in Sports and Exercise, 33(3), 413–421. https://doi.org/10.1097/00005768-200103000-00013
Neufer, P. D. (1989). The effect of detraining and reduced training on the physiological adaptations to aerobic exercise training. Sports Medicine (Auckland, N.Z.), 8(5), 302–320. https://doi.org/10.2165/00007256-198908050-00004
Pope, Z. K., Willardson, J. M., & Schoenfeld, B. J. (2013). Exercise and blood flow restriction. Journal of Strength and Conditioning Research, 27(10), 2914–2926. https://doi.org/10.1519/JSC.0b013e3182874721
Renzi, C. P., Tanaka, H., & Sugawara, J. (2010). Effects of leg blood flow restriction during walking on cardiovascular function. Medicine and Science in Sports and Exercise, 42(4), 726–732. https://doi.org/10.1249/MSS.0b013e3181bdb454
Silva, J. C. G., Domingos-Gomes, J. R., Freitas, E. D. S., Neto, G. R., Aniceto, R. R., Bemben, M. G., Lima-Dos-Santos, A., & Cirilo-Sousa, M. S. (2021). Physiological and Perceptual Responses to Aerobic Exercise With and Without Blood Flow Restriction. Journal of Strength and Conditioning Research, 35(9), 2479–2485. https://doi.org/10.1519/JSC.0000000000003178
Staunton, C. A., May, A. K., Brandner, C. R., & Warmington, S. A. (2015). Haemodynamics of aerobic and resistance blood flow restriction exercise in young and older adults. European Journal of Applied Physiology, 115(11), 2293–2302. https://doi.org/10.1007/s00421-015-3213-x
Tegtbur, U., Haufe, S., & Busse, M. W. (2020). [Application and effects of blood flow restriction training]. Der Unfallchirurg, 123(3), 170–175. https://doi.org/10.1007/s00113-020-00774-x
Wei, J., Nassis, G. P., Gu, Z., Zou, Y., Wang, X., & Li, Y. (2021). Acute physiological and perceptual responses to moderate intensity cycling with different levels of blood flow restriction. Biology of Sport, 38(3), 437–443. https://doi.org/10.5114/biolsport.2021.100146
Wiegand, K., Mercer, J. A., Navalta, J. W., Pharr, J., Tandy, R., & Freedman Silvernail, J. (2019). Running status and history: A self-report study. Physical Therapy in Sport, 39, 8–15. https://doi.org/10.1016/j.ptsp.2019.06.003
Author and Mentor Bios
Violet Sullivan will graduate in spring 2023 with a bachelor of science degree in exercise science and a minor in chemistry. She is a member of multiple honors societies, including the University Honors Program, and is part of the Hamel Scholars Program. Originally from Brentwood, New Hampshire, Violet is on the UNH cross country and track and field teams. She was able to combine these interests into her Honors senior thesis project by working with Summer Cook, associate professor of kinesiology at UNH, to study the impact of running with blood flow restriction, funded by a Student Undergraduate Research Fellowship (SURF). Dr. Cook is a leading researcher in this area, allowing Violet to design and conduct cutting-edge research on this technique that could potentially be used for training and rehabilitation in the future. Violet loved the teamwork aspect of conducting human subjects’ research in the exercise science lab and is thankful for the help of Research Experience and Apprenticeship Program (REAP) recipient, Amanda Ares, in data collection. Overseeing this research project start to finish will be helpful for Violet’s future goal to attend medical school, where she is currently most interested in specializing in nonsurgical sports medicine. She is excited to share more about her research with the broader UNH community through Inquiry.
Summer Cook is an associate professor in the Department of Kinesiology at the University of New Hampshire, where she has been since 2009. Her research focuses on improving human performance, particularly neuromuscular function through blood flow restricted exercise, in young adults, athletes, and older adults. Dr. Cook has served as a research mentor to over twenty different students who were awarded funding through the Hamel Center for Undergraduate Research. She has been mentoring and conducting research with Violet for over three years. They combined interests to develop Violet’s project to investigate the use of blood flow restricted exercise in competitive female runners, and Dr. Cook enjoyed seeing Violet act as an independent researcher for this project. She describes Violet as an extraordinarily skilled researcher who is precise, always follows protocols, and is also good at troubleshooting problems when they arise—one of the best undergraduate student researchers she has worked with at UNH. In Dr. Cook’s view, writing for Inquiry lets undergraduate student researchers be more creative and responsive to what may excite readers, and makes students work hard to translate their research into understandable and meaningful results for readers not in their fields.
Copyright 2023, Violet Sullivan
